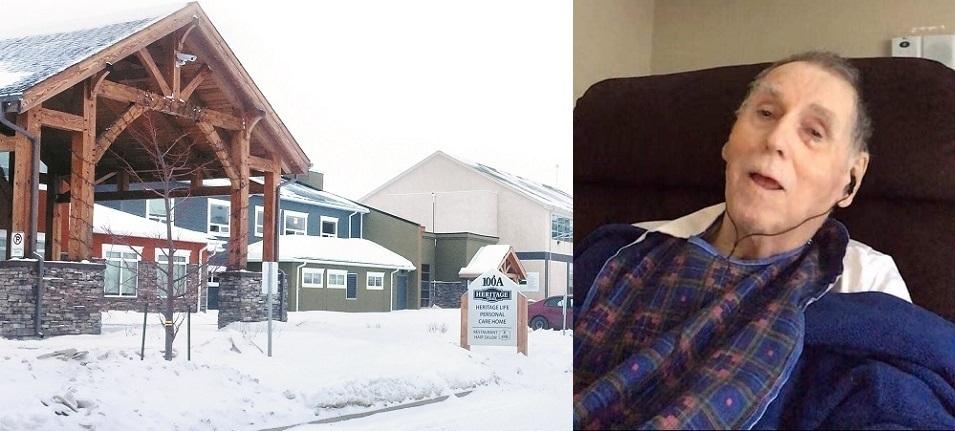
The COVID-19 outbreak at the Heritage Life Personal Care Home in Niverville remains active. The first case, a staff member, was reported to the public on January 4. As of the most recent update from management, made available on February 17, there have been a total of 51 cases, of which 38 have been residents. Nine residents have passed away. Thirteen staff members have also tested positive for the virus.
Before the outbreak, there were 80 residents in the PCH, meaning that approximately 48 percent of the residents have by now contracted COVID-19 and 11 percent have passed away.
The first vaccine dose has been completed for residents and the second dose had been scheduled for February 18. A good number of staff are being vaccinated as well.
Up until their February 9 update, the PCH had been reporting that the cases remained confined to two neighbourhoods, Prairie Rose and Lilac Lane. However, the updates since that time no longer make this assertion.
“Our staff have worked quite hard at monitoring our residents, as well as any crossover between all of the neighbourhoods,” says CEO Wes Hildebrand.
Hildebrand declined to clarify whether recent cases have cropped up in other neighbourhoods.
One Niverville resident with a fair bit of experience with the PCH has concerns about the situation. Stephan Geissler’s grandfather, Egon Meyer, resided at Heritage Life for three years before passing away from COVID-19 in January. During that time, Geissler got to know many of the residents and staff.
“The nurses and healthcare aides do tremendous work, but in my opinion are overworked and understaffed across the board,” says Geissler. “It is my understanding that on overnight shifts, there is only one nurse for 80 residents. If you have multiple residents who fall ill overnight, the quality of care becomes severely compromised because one nurse can’t reasonably attend to multiple sick patients at the same time. Healthcare aides do what they can within their authority, but it’s a delicate balance as some people require more care than others, such as two-person assists.”
Geissler wonders how one or two support staff can manage all this, given that some residents have dementia and tend to wander throughout the facility.
“Mealtimes used to be group activities,” he says. “How do two staff and one nurse ensure that residents can safely eat their meals? A lot of residents require assistance or are at risk for choking. I just don’t think the resources are there.”
Hildebrand addressed the question of staffing. “Heritage Life Personal Care Home has always met the staffing contingent that is required by our provincial government,” he says. “Our residents are being served and are eating in their own neighbourhoods. In outbreak neighbourhoods, the residents eat in their rooms.”
Nonetheless, Geissler says that on a few occasions his grandfather was left without water that he could reach, or he was stuck waiting for help to either get to the washroom or out of the washroom.
“It’s difficult to have those conversations with your loved one and try to explain why that’s happening, because the concerns are legitimate and frustrating and they’re the ones living it,” Geissler says. “We know everyone tried to do their best, and it’s what you can expect when the staff levels are the way they are and fresh faces who don’t know the residents join the fold. I don’t think this is a reflection on the staff so much as it’s a reflection on the province for underfunding care homes and creating a work situation that is very emotionally and physically draining on both staff and residents. Our most vulnerable citizens deserve the best care in their final years.”
Geissler was a designated caregiver for his grandfather, but with that responsibility came a stipulation: if an outbreak occurred at the PCH, designated caregivers could be required to care for their loved one under the supervision of the staff.
Geissler was unable to accept that responsibility in its entirety because he has pre-existing medical conditions.
“It’s a shady thing to ask someone to come in and do that, a family member with no medical training, placing themselves at risk by entering a hotbed of COVID-19 to care for their loved one because the government failed to protect them,” Geissler says. “I just felt like this was desperate and a non-plan.”
Fortunately, Geissler and his family were able to communicate with Meyer via iPad and phone conversations.
“At times there have been directives from Public Health to stop or restart visitation,” says Hildebrand. “The designated caregivers are a key part of the care plan for all our residents.”
Geissler feels that the staff of the PCH did their best overall, but he thinks the board may not have fully explored other models of care that have proven to be successful.
Early in the outbreak, Geissler and his mother expressed their concern to management that the chosen approach, which allowed for indoor visitation, could lead to more airborne transmission of the virus. They were also concerned that other families might breach protocols during visits.
They suggested moving towards supervised and distanced visits, which were more common during the pandemic’s first wave. He says that management chose to remain focused on the residents’ mental health and the effects of isolation.
“It’s a tough situation,” Geissler says. “We do feel that there were reasonable options to hold visits and reduce the risk of exposure.”
Despite everything, Geissler saw staff members going above and beyond to care for his grandfather and the other residents. He believes these staff were exhausted and overworked and yet still gave of their time, and their love, to those who needed it so desperately.
Although Egon Meyer died in January, Geissler says that his wish was to see change happen in the PCH to allow for more person-centred care and for the province to acknowledge its failures in terms of offering good quality of life for those transitioning from independent living to round-the-clock care.